By Liao Zhe-min
Translated by Wu Hsiao-ting
Photos by Hsiao Yiu-hwa
Former COVID patients share their experiences and healthcare professionals share tips to help people recover from long COVID.

When a surge of COVID cases caused by the Omicron variant began to subside in June 2022, people in Taiwan started appearing in public places more often, learning to coexist with the virus.
In mid-May this year, Mr. Wu, an office worker in Taipei, northern Taiwan, arrived home from work feeling under the weather. He had difficulty swallowing and was running a fever. He took a rapid COVID test—for which he tested positive—before going to the hospital the next day for a PCR test. The PCR test also came back positive.
“It was like I had suffered lacerations in my throat,” Wu said of his COVID symptoms. “I could barely speak. My throat hurt when I ate as well.” He felt like he had fallen victim to an extremely brutal cold or flu. His symptoms lasted for about four days.
He used throat lozenges, over-the-counter medicine, and health supplements while he was isolating at home. He also drank two liters of water a day. “I felt I had recovered after a week, but I noticed that my stamina had declined. I became tired more easily. I had a couple of coughing fits every day, and sometimes suffered from shortness of breath.” To nurse himself back to health, he decided he’d exercise more often and keep healthier hours.
Ms. Chen, 51, also tested positive for COVID-19 in May. Like Mr. Wu, she noticed a decline in her stamina after she recovered. She found she needed more frequent rests. She also had a lingering cough. After the experience, she concluded: “COVID-19 is not your typical cold or flu after all. I felt like the virus had run amok in my body, attacking all the vulnerable places in me.”

People in Taiwan line up to have PCR tests at a hospital. COVID cases spiked in April and May in 2022, straining hospital resources as well as the supply of rapid test kits.
Even when you recover
Compared with the Alpha and Delta variants, people testing positive for the Omicron variant have experienced reduced chance of severe illness and death. In fact, over 99 percent of those infected with this variant reported mild or no symptoms at all. In spite of those positive numbers, some people have lingering symptoms, even months after they’ve recovered from the disease itself.
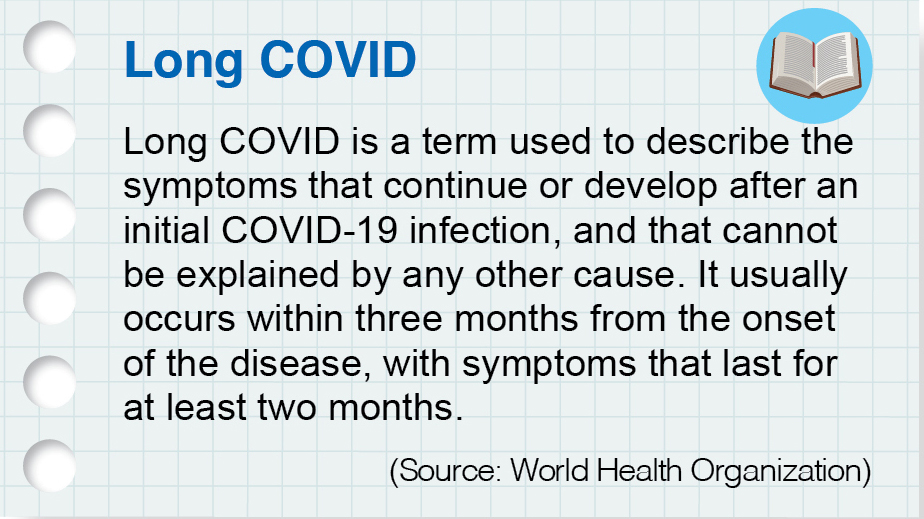
The World Health Organization established a clinical case definition of post-COVID-19 condition in October 2021: “Post-COVID-19 condition [or long COVID] occurs in individuals with a history of probable or confirmed SARS-CoV-2 infection, usually 3 months from the onset, with symptoms that last for at least 2 months and cannot be explained by an alternative diagnosis.” Common symptoms include respiratory system disorders, hair loss, rashes, depression, anxiety, difficulty sleeping, heart palpitations, chest pain, and cognitive dysfunction (brain fog).
Dr. Chang En-ting (張恩庭), a specialist in thoracic medicine at Hualien Tzu Chi Hospital, eastern Taiwan, explained that the coronavirus can attack cells all over your body, triggering an immune response and causing inflammation in your body. When the acute phase ends, a patiently gradually recovers, but in some cases, the inflammation does not disappear entirely. This is referred to as chronic inflammation.
A UK study published in The Lancet Respiratory Medicine in April this year tracked a total of 2,320 COVID patients discharged from their hospitals between 2020 and 2021. Two-thirds of the patients felt they had not fully recovered, even up to one year after discharge. People suffering from worse aftereffects even developed more severe inflammation than before.
A person’s likelihood of developing long COVID is not linked to the severity of the initial infection. In fact, people with mild and severe symptoms can suffer from lingering health problems. According to the American Medical Association, there are three types of long COVID. The first category includes people who have ongoing symptoms due to direct cell damage from the virus. The second is when one’s symptoms are linked to chronic hospitalization, such as muscle weakness. The third category covers those cases in which symptoms appear after recovery.
Mr. Ye tested positive for COVID-19 in 2021, and recovered after ten days of treatment in isolation at a hospital. However, after he was discharged, “all kinds of aftereffects of the disease surfaced,” he said, “such as chest pain, coughing, poorer sleep quality, and poorer memory.” He added with dismay that sometimes he even forgot he was boiling water and had scorched two pans as a result. There were also instances on which he forgot to take his purchases home from the store after paying for them.
In order to return to his former healthy self, Ye adjusted his diet by becoming a vegetarian. He also did chest expansion exercises regularly, and rode his bicycle in the afternoons. He also made sure to drink plenty of water, and used an oximeter to monitor the level of oxygen in his blood. “I’ve become more health-conscious,” he said, which was probably a positive aftereffect of the disease.

People who have recovered from COVID-19 should get exercise and maintain interactions with others to help their lives return to normal.
Healthy routine and diet
Dr. Chang En-ting said that the first order of business as we learn to coexist with the coronavirus is to avoid being infected. He advised taking precautionary measures and getting immunization shots, which is an effective way of reducing the likelihood of severe illness. Among those who have been infected and have recovered, the doctor has encountered some who still have shortness of breath, become tired more easily, or have a lingering cough with phlegm. He works first to reduce the inflammation in such patients, then works to eliminate their phlegm. If their conditions improve, he helps them improve their cardiopulmonary function. He instructs such patients to do aerobic exercises for at least 30 minutes a day. Exercises such as walking or tai chi will do as well.
Dr. Shen Huan-ting (沈煥庭), who heads the division of thoracic medicine at Taichung Tzu Chi Hospital in central Taiwan, advises against chilled drinks. He said that chilled drinks can lead to the contraction of the bronchus and exacerbate coughing.
COVID-19 can affect not just one’s physical health, but one’s psychological well-being as well. Ms. Zeng was diagnosed with the infection last year. Her condition took a turn for the worse when she was being treated in the hospital. She eventually was transferred to an intensive care unit. When she had recovered, people around her suggested that she go out to thank the medical workers and other people who had helped her along the way. But she felt as if a dark cloud was still hanging over her. She couldn’t bring herself to leave her home, not even two months after she was discharged from the hospital. The experience of contracting the disease had instilled fear in her. “It’s dangerous outside,” she thought. “What if I get infected again?” Fortunately, her friends’ company and her increased exposure to Buddhism eased her mind and changed her way of thinking: “I’ve regained my health,” she told herself. “When would there be a better time than now to go thank those who have helped me?”
It’s not just the body that needs healing after COVID, but the mind as well. Receiving care from others is even more important if your mind “falls ill.” Dr. Chaucer C.H. Lin (林喬祥), the director of the Psychotherapy and Counseling Center at Hualien Tzu Chi Hospital, pointed out that some recovered COVID patients suffer from post-traumatic stress disorder and might exhibit symptoms of inattention, anxiety, and depression. Contributing to this is that they haven’t fully returned to their old routines yet.
Dr. Lin explained that most people infected with COVID are required or choose bed rest during their treatment or recovery periods. As a result, they keep very different hours than before. The first thing to do after recovering is therefore to try to return to your familiar, regular routine. You can also learn to relax in ways that feel comfortable for you. Taking deep breaths, meditating, or chatting or interacting with friends are all good ways to calm your mind or relieve your stress.
At the end of 2021, Taiwan’s National Health Insurance Administration launched a healthcare program for people who have recovered from COVID-19 but still suffer from ongoing symptoms. People can check with hospitals in their area to see if they participate in this program, which integrate services in thoracic medicine, infectious diseases, psychiatry, rehabilitation, nutrition, and so on. They can then seek help accordingly.
According to a study carried out by the Faculty of Medicine at the Chinese University of Hong Kong (CU Medicine) and published early this year in the medical journal Gut, the composition of gut microorganisms in people infected with COVID is very different from that in uninfected individuals and is related to disease severity. “COVID-19 patients lack certain good bacteria known to regulate their immune system and the abnormal gut microbiota [dysbiosis] persists after clearance of the virus, which could contribute to lingering symptoms,” said the CU Medicine website. The gut is the largest immune organ in the human body; 70 percent of the immune system is located there. A healthy balance of gut bacteria is therefore important and a proper diet is essential to maintaining it. Dietician Su Zhen-ying (蘇真瑩) of Hualien Tzu Chi Hospital suggested trying a whole-food, plant-based diet. (For more about this vegetarian diet, please read our November 2021 issue.) As for those who are not used to a vegetarian diet, she suggested a Mediterranean diet. Such a diet is high in vegetables, legumes, nuts, fruits, and olive oil and low in red meat and dairy products. Rich in dietary fiber, the diet promotes gut health and helps build a healthier immune system.
Dietician Su has designed a set of guidelines to help former COVID patients promote a healthier gut and improve their health. The chart is included at the end of this article for reference.
 Zoom in picture)
Zoom in picture)

